“The nation is in the midst of the longest recession since the Second World War. While healthcare has historically been less vulnerable to economic downturns than other industries, Florida hospitals are feeling the financial pain of today’s struggling economy.”
Florida Hospital Association April 2010
A tragic car accident, a medical emergency in the middle of the night, a child with a high fever, and we never give a thought that our medical facilities may not stand ready and able to help us. Everyday we hear news about changes in healthcare, but we rarely give a second thought as to how it could affect us.
 Providing medical care is a business. As much as we would like to believe that the delivery of medical care is somehow above other business models, the reality is that if medical providers are not profitable, they cannot remain in business.
Providing medical care is a business. As much as we would like to believe that the delivery of medical care is somehow above other business models, the reality is that if medical providers are not profitable, they cannot remain in business.
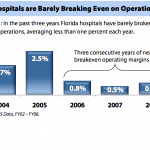
As you can see in the graphic above, operating margins for hospitals in Florida are across the board in a steady decline. Certainly the number of people who utilize the medical systems have increased however, the cost of providing care is also steadily increasing. Facilities that provide medical care are forced to keep up with technological advancements, medical procedure advancements and a higher cost of maintaining a qualified workforce. Like most large businesses, the medical corporations are forced to make capital investments in facility, equipment and stock portfolios. Just as the Nation has been struck with a stock market decline and increased cost of borrowing, so have the corporations been affected adversely. A secondary challenge for hospital providers, are a rapid rise in unfunded or “self-pay” care. The rising increase in job loss, currently at 11.9%, has caused many people to lose their healthcare coverage. The Florida Hospital Association study shows that “20.2% of Floridians lack health insurance, compared to the national average of 15.4%.” When an unfunded patient suffers an illness or accident, the patient still receives the highest level of medical care possible. Clearly when hospital bills are tens of thousands of dollars, even for a minor event, no one is able to pay for this unfunded care. Another challenge is that an aging population is reliant on Medicare, which according to an April 2010 Florida Hospital association:
“In 2002 Medicare reimbursed at 96.5 percent of cost, meaning that hospitals received 96 cents for every dollar of care provided. In 2008 Medicare reimbursement as a percent of cost declined to 91.1 percent. Medicaid reimburses at an even lower rate, but the rates vary significantly in Florida depending on whether the hospital is exempt from rate controls. In 2008, Florida hospitals received 86 cents for every dollar of care provided to Medicaid patients. Florida hospitals that are not exempt from Medicaid rate controls received only 56 cents for every dollar of care provided. Statewide, over half of the care provided in Florida hospitals is delivered to Medicare patients; there was a slight decline from 53.2 percent of all patient days in 2002 to 51.2 percent of patient days in 2008. At the same time, the percent of Medicaid patients cared for at Florida hospitals has increased, from 13.9 percent in 2002 to 16.6 percent in 2008.”
Possibly the most challenging and alarming challenge to our society is trauma care. Trauma care is much more expensive to provide, due to the cost of staffing trauma centers with 24 hour access to specialty care providers such as trauma surgeons, neurological surgeons and pediatric specialists. According to a May 2004 white paper published by National Foundation for Trauma Care, “Trauma centers collectively experiences a $1 billion dollar loss, and with increased costs, this problem will worsen over time.” This study lists increasing number of unfunded patients, a failure of the previously used modality of “cost-shifting,” problematic relationships with managed care, poor reimbursement of Medicaid patients and decreasing auto insurance reimbursement. These factors are troubling, as trauma care is a well-respected life saving advancement in the last 30 years. Conservative estimates and historical evidence shows that if this trend continues, “current rates of closures among the nation’s 600 trauma centers will increase and 10-20% (of trauma centers) will close within the next 3 years.”
The image of a “closed trauma center” is frightening, especially when estimates show there are 687,000 injured Americans that utilize this care annually. The unfortunate cascade of a trauma center closure, is that the expensive cost of saving lives would then be passed to a secondary and less prepared medical provider who is certainly not capable of absorbing these costs and will close shortly after. The human cost is the most important factor affected by the hospital closure, but what about the economic impact that states will suffer? The Florida Hospital Association study demonstrates that, “one quarter of a million Floridians are employed by Florida hospitals. This makes hospitals one of the largest single employment sectors in Florida’s economy.” “$32 billion dollars in wages and salaries were attributed to Florida hospitals in 2007.” “$80 billion dollars is the estimated total economic impact Florida hospitals have on the state’s economy.” Clearly what is good for health care, is good for Florida.
 The following graphic shows States that are at risk of closure:
The following graphic shows States that are at risk of closure:
Unfortunately we live in a State that is in “high-risk.”
Consider also that our medical care providers, especially trauma care providers, are facilities we count on for any potential trauma encountered by future terrorist attacks. The 1995 Oklahoma City Bombing caused 759 total casualties, 162 immediate deaths and 83 hospitalized patients, 52 of who were critical. Attacks of this scale would challenge even the most intact medical system. A system that is in “critical condition” currently would certainly be threatened by any natural or man-made disaster. The trade-off is either cost containment or decreased quality in care provided, neither of which will be well tolerated by our citizens.
The “Obama Healthcare Plan,” is in principal, designed to provide coverage to everyone. As with most very complicated systems, the devil is in the details. Certainly the medical system would benefit from a decrease in unfunded care, but the question remains if the systems themselves would be better off fiscally.
An August 30th, 2009 article, Washington Post writer, Peter Slevin, Hospital Executives Worry About the “What-If’s” of Reform, quotes hospital network CEO Charles J. Barnett, “Any savings beyond this agreed-to amount would harm hospitals’ ability to provide the care their communities need,” the American Hospital Association said in talking points to members, including nearly 5,000 hospitals and health networks. The document noted “serious concerns” about House legislation that includes a government-run plan competing with private insurance.”
Currently medical care protocol is not forced upon physicians and hospitals however, if they hope to be reimbursed for this care, they are forced to comply. Given the fact that “healthcare reform” is a large government designed program, the methods of healthcare delivery may indeed be influenced by funding.
In contrast to “socialized healthcare” delivered in other countries, we currently have a level of technology that would be difficult to recede from. Our standard of care is at a level that we have come to expect for the most part and would rebel if access to care and testing were decreased.
The usual example of “socialized care” is that it may take 6-months to get a minor surgery that in the U.S. we would have much more rapid access to. This systemic approach usually divides society into “the haves and have-nots.” Another drawback to “socialized care” is the difficulty to recruit and retain physicians who are limited in their income by the state’s utilization policy. Fortunately our healthcare reform is not patterning itself on the true “socialized care” model. We may however, experience some of the same challenges.
The challenge of providing healthcare to the American people is certainly complicated. We all agree that in a perfect world, we would always have the basic right of healthcare. The ultimate disconnect is that we are unable to afford this access to care. Healthcare reform is greatly needed and universally welcomed. We simply need to educate ourselves as to what system will fulfill the greatest good for the greatest number of citizens. The first step is the realization that someone must pay for this care. The second step is that we must all do our part, when possible, to keep healthy and safe. Just as in any corporate structure, hospitals and medical providers must have a healthy fiscal outlook as well as learning to adapt more rapidly to the changes in our social demographic and needs.


